Since the beginning of the pandemic, the world has relied heavily on two main types of tests to detect COVID-19. There’s the molecular (RT-PCR) test that identifies the presence of the virus’s genetic material, and the serological antibody tests that look for specific antibodies made by the immune system in response to the virus.
There are numerous advantages and disadvantages to both; you can find those details in a previous blog post located here.
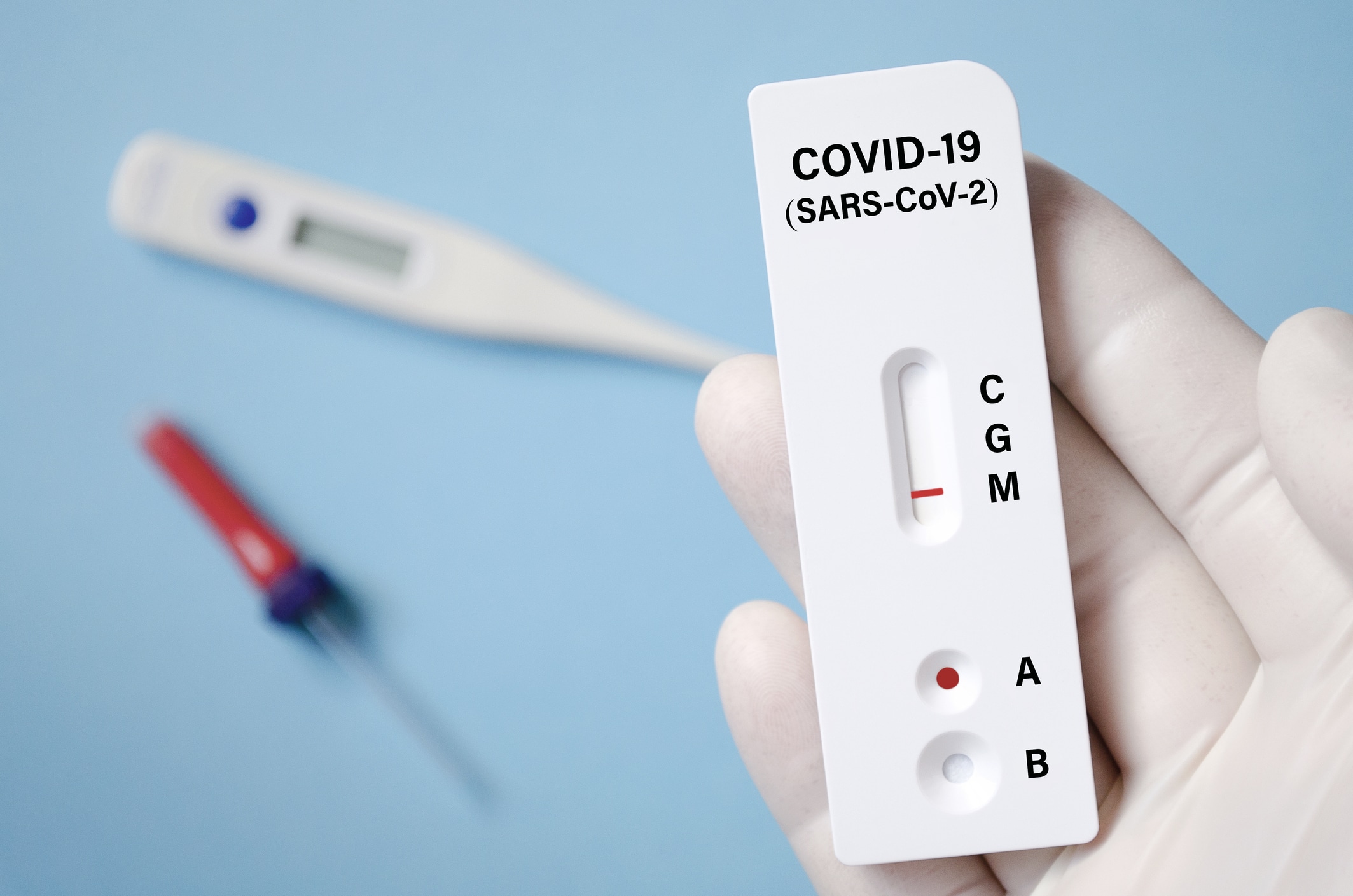
In recent months, a third test has come on to the scene, and it’s rapidly gaining popularity due to its middle-of-the-road characteristics and low price point.
How it worksÂ
The rapid antigen test is similar to the molecular (RT-PCR) test because it is diagnostic and determines if one has an active coronavirus infection, but it differs in its mechanism of detection.
The rapid antigen test detects specific proteins that live on the virus’s surface instead of looking for the virus’s genetic material like the molecular (RT-PCR) test. Once a sample is collected, via nasal/throat swab or saliva, it can be mixed with a solution that breaks open the virus and releases specific and easily detectable viral proteins.
As a result of this alternative mechanism for detecting the virus, you do not have to process antigen tests in a lab. Instead, the tests can produce results in less than 30 minutes.
Disadvantages
While the faster processing time is a great advantage, there are still some disadvantages to antigen testing.
- A big drawback is its sensitivity or rate of detecting coronavirus infections correctly.
- A typical PCR test can detect a single molecule of RNA in a microlitre of solution
- Antigen tests need a sample to contain thousands to tens of thousands – of virus particles per microlitre to produce a positive result.
These disadvantages mean that those with lower amounts of the virus in their bodies may go undetected, or that inadequate specimen collection may also result in false negatives. Basically, the test could say that someone doesn’t have the virus when they actually do have it.
Ongoing Debate
Despite the rapid antigen test’s comparatively lower sensitivity, some have argued that it may be advantageous in the context of a global pandemic. Researchers have found that the viral load peaks early in COVID-19 infections and then gradually declines, with only tiny amounts of the virus remaining in someone’s nose or throat.
And although there is not enough data to equate different viral levels with how infectious people are, there is evidence that individuals are unlikely to spread the virus about eight to ten days after showing symptoms.
So this type of test could detect the virus early in the cycle, potentially when people are the most likely to spread the disease. From an epidemiological standpoint, antigen testing could be a good tool.
Slowing the Outbreak?
Implementation of a rapid antigen test into a point-of-care testing strategy may help to limit the spread of the virus. People with high levels of the virus may be more likely to transmit it to others, but these individuals may be more easily identified through rapid antigen testing due to their higher viral load.
On the other hand, some experts caution that infected individuals with lower levels of the virus, who may be harder to identify, may still have the potential to transmit the virus to others. People in this group may feel a false sense of security from a negative rapid antigen test, while still posing a risk for transmission.
The Private Sector
In the private sector, many organizations are working to protect their employees across a wide array of public responses. Rapid antigen testing could prove to be the most cost-effective and impactful solution available for this group if used appropriately.
Antigen testing is one of the many tools available. The gold standard for high sensitivity and accurate results is still PCR testing. This is why PCR testing is still common even though antigen testing is more cost-effective and timely.
Dealing with the False Negatives
A plan that relies solely on antigen testing must have processes in place for dealing with the false negatives, such as requiring employees to take more than one test.
High-frequency testing and effective mitigation techniques may be combined to provide a viable solution for mitigating coronavirus.
In the constantly changing environment of a global pandemic, it is critical to have a medical expert help develop your coronavirus mitigation plan.
How RMI can help with Antigen testing
Despite its potential utility, there remain unknowns about the procurement and efficacy of antigen testing. As a result, Remote Medical International (RMI) is not currently offering antigen testing to our clients. However, as the technology progresses and new tests become available, this may quickly change.
Through RMI consulting, you can stay up-to-date on the latest advancements and when the time comes, implement antigen testing into your COVID-19 testing strategy.